Quick Answer
Traumatic brain injury (TBI) presents a profound legal and personal challenge. Traumatic brain injury lawyers specializing in TBI cases must navigate medical complexity, long‑term disability consequences, and nuanced liability theories.
If you or someone close to you has suffered a traumatic brain injury (TBI), it can feel like your entire world has been turned upside down.
On top of the pain and recovery, you're left trying to make sense of complicated legal and medical systems.
This guide is here to walk you through what TBIs are, how they happen, what your legal options are, and how the right legal assistance can help.
How dangerous are TBIs?
A traumatic brain injury isn’t just a bump on the head. It can change a person’s life in an instant.
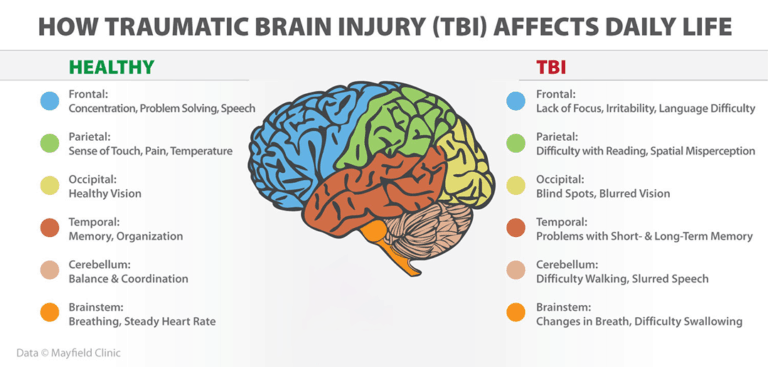
Depending on severity, it can lead to memory loss, mood changes, difficulty speaking or walking, or even long-term disability.
Here are a few facts:
- Around 2.9 million Americans end up in the ER, hospitalized, or die each year because of a TBI.
- 223,000 people were hospitalized for TBIs in 2019 alone.
- Every year, about 70,000 people die from TBIs in the U.S.
Many people think concussions are minor, but even a "mild" TBI can cause long-term problems.
For example, someone who had a minor car crash might seem okay at first but then struggle with headaches, memory issues, or irritability for months.
Globally, 50–60 million people sustain a TBI annually, costing approximately $400 billion per year1 (NCBI).
Severity strongly predicts outcome.
Mild TBIs make up over 90% of diagnosed cases while moderate and severe cases carry higher risk of long‑lasting disability or death.
Mortality sits at about 21% by 30 days post‑injury2, with severe combat‑related TBI mortality up to 30–50%.
Roughly 10% of mild injuries, 66% of moderate, and nearly all severe cases result in permanent disability.
What are the major causes of traumatic brain injuries?
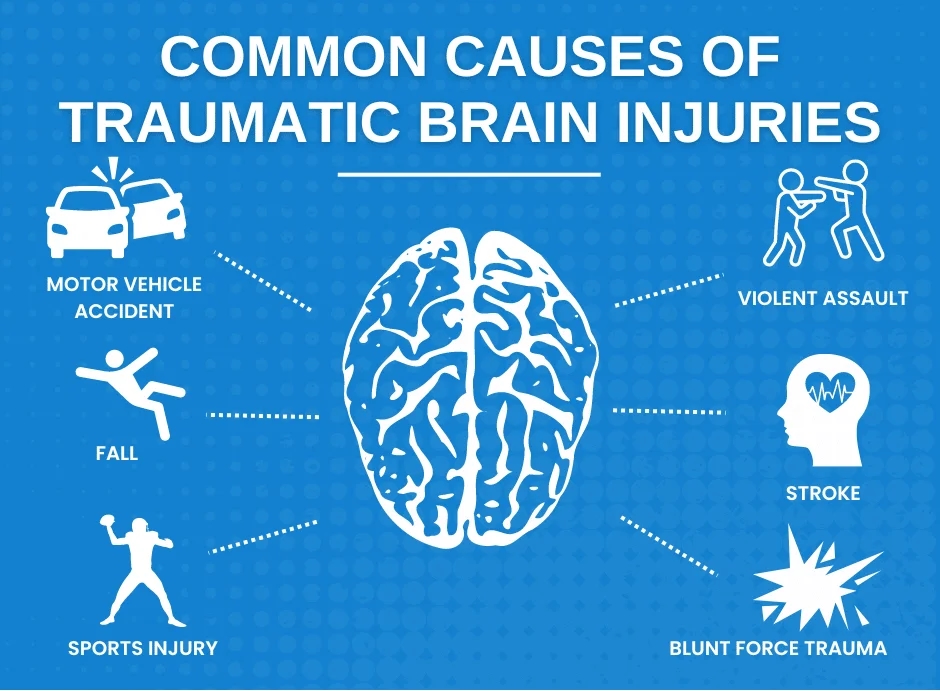
According to CDC and related sources, causes are:
- Falls (~32–35%)
- Vehicle crashes or car accidents (~17%)
- Being struck by or against an object (~16.5%)
- Assault (~10%)
- Other or unknown (~21%).
Sports injuries account for 1.6–3.8 million TBIs annually in U.S. sports and recreation alone.
Violence, birth trauma, workplace accidents, and firearms are also prominent causes.
Car accidents
Motor vehicle collisions generate rapid acceleration‑deceleration and impact forces, causing coup‑contrecoup injuries and diffuse axonal injuries (DAI).
DAI is typical in high‑speed crashes, resulting in nerve fiber shearing and often prolonged loss of consciousness or coma.
Even at speeds under 30 mph, a crash can cause your brain to jolt inside your skull. You don’t even need to hit your head to suffer TBI, just a sudden stop can do damage.
Imagine someone rear-ending your car. Your body goes forward, then snaps back.
That motion alone can injure your brain.
Serious falls
Falls account for about a third of all TBIs. Children under age 4 and adults over age 75 are at highest risk from falls.
In older adults, altered balance and bone fragility increase both incidence and severity.
Picture someone slipping on a wet supermarket floor, hitting their head, and ending up with a brain bleed.
That’s more common than you might think.
Birth injuries
Sometimes babies suffer from TBI during delivery. This can happen if a doctor uses forceps incorrectly, waits too long to perform a C-section, or fails to notice the baby isn't getting enough oxygen.
These injuries can lead to lifelong challenges for the child and heartache for the family.
Birth‑related TBIs result from prenatal hypoxia, forceps or vacuum extraction misuse, or negligent monitoring.
In infants aged 2–4 falls and traffic injuries also contribute.
Birth hypoxia and shaken baby syndrome represent legally sensitive and medically complex causes of TBI.
In medical malpractice cases, proving causation requires expert testimony about deviation from obstetrical standards, timely intervention, and the nature of oxygen deprivation or trauma.
Bicycle accidents
Cyclists are vulnerable to high‑velocity impacts with motor vehicles, fixed objects, or falls.
Head injuries often involve blunt force trauma leading to closed‑head TBIs or DAI.
Liability may extend to distracted drivers, unsafe road conditions, defective bicycle design, or inadequate infrastructure such as missing bike lanes or signage.
Medical malpractice
Not all TBIs are caused by accidents. Sometimes doctors make mistakes, like missing a brain bleed after a fall or not giving enough oxygen during surgery.
These errors can lead to lasting damage.
Negligence in medical settings can result in iatrogenic TBIs during surgery, anesthesia errors, delayed diagnosis of bleeding, or failure to monitor intracranial pressure.
A missed subdural hematoma or low oxygen event can cause secondary injury, complicating legal claims.
Claimants must work with neurologists and neurosurgeons to establish breach, causation, and damages.
Sports and recreational accidents
Contact sports lead to high rates of concussion and repeat injury. In high school and college athletics, nearly 300,000 athletes sustain TBIs annually.
One hard hit in football or a poorly placed header in soccer can cause a concussion. And if someone’s sent back to play too soon, another hit could do even more harm.
Concussions are considered mild TBIs but repeated episodes can lead to chronic traumatic encephalopathy (CTE) or persistent cognitive problems.
Legal claims may focus on unsafe equipment, failure to remove injured players, inadequate protocols, or misrepresentation by leagues.
Head trauma in other contexts
This includes shaken baby syndrome, violent assaults, work‑related head injuries, falls from height or scaffolding, and blast injuries.
- Assault and child abuse constitute a significant portion of pediatric TBIs.
- Child abuse causes about 19% of pediatric brain trauma.
- Workplace TBIs account for about 60% of head injury claims in workers’ compensation3.
Different types of brain injuries
Brain injuries can take many different forms, each with their own level of severity and risk for lasting complications.
Below are several distinct types that highlight just how varied the effects of head trauma can be:
- Concussions: Often referred to as mild traumatic brain injuries (mTBIs), concussions affect brain function after a blow to the head or sudden jolt that causes the brain to move inside the skull. They don’t always involve loss of consciousness, which makes them easy to overlook, even after what seems like a minor knock.
- Minor head injuries: The area between the scalp and skull is filled with blood vessels that can easily bruise or swell after impact. These injuries may result in noticeable bumps or discoloration and often respond well to cold compresses, though it’s wise to seek medical advice after any head trauma.
- Hematomas: This injury involves a collection of blood outside of blood vessels, often forming a clot. When this occurs within the skull, it can create pressure against the brain tissue, potentially leading to serious damage if untreated.
- Edema: Swelling inside the brain can be life-threatening because the skull is a fixed space. As fluid builds up, pressure increases and can impair brain function or destroy healthy tissue.
- Hemorrhages: These are instances of active bleeding either within the brain itself or in the surrounding areas. Depending on location and volume, a brain hemorrhage can rapidly become critical.
- Diffuse axonal injury (DAI): One of the more severe forms of TBI, DAI, happens when the brain is forcefully rotated or shaken, tearing nerve fibers across large areas. This type of injury can disrupt brain communication and often results in coma or significant long-term impairment.
- Hypoxic and anoxic brain injuries: These occur when the brain is deprived of oxygen—partially (hypoxia) or completely (anoxia). They may result from incidents like cardiac arrest, near-drowning, suffocation, or medical emergencies, and can lead to widespread cognitive or physical decline.
- Second impact syndrome: Though rare, this condition is extremely dangerous. It occurs when someone experiences a second head injury before fully recovering from an earlier concussion. The result can be sudden, massive brain swelling with catastrophic outcomes.
No matter the type, brain injuries should always be taken seriously even when symptoms are subtle or delayed.
Damage can be significant without any outward signs, which is why early assessment and intervention are so important.
Common brain injury symptoms
Not all brain injuries look the same, and symptoms can range from barely noticeable to completely life-altering.
Some show up right away, while others might take hours or even days to appear.
Here are the most common signs to watch for:
Physical symptoms:
- Headaches: Persistent or worsening pain following an impact.
- Dizziness or balance problems: Feeling unsteady when standing or walking.
- Nausea or vomiting: Especially common in the hours immediately after injury.
- Blurred or double vision: Visual disturbances or sensitivity to light.
- Fatigue or drowsiness: A strong need to sleep or difficulty staying awake.
- Loss of consciousness: Even a few seconds of blacking out can indicate serious trauma.
- Seizures: May occur shortly after injury or later as a complication.
Cognitive symptoms:
- Confusion or disorientation: Not knowing where you are or what just happened.
- Memory issues: Difficulty recalling events before or after the injury.
- Trouble concentrating: Feeling mentally foggy or easily distracted.
- Slow thinking: Tasks that were once easy may feel mentally exhausting.
Emotional and behavioral symptoms:
- Irritability or mood swings: Sudden changes in attitude or personality.
- Depression or anxiety: Emotional shifts that don’t seem tied to anything specific.
- Lack of motivation: Difficulty starting or completing everyday activities.
- Sleep disturbances: Insomnia, oversleeping, or irregular sleep cycles.
Sensory symptoms:
- Ringing in the ears (tinnitus): Often reported after concussions.
- Changes in taste or smell: A dulling or loss of senses.
- Light and sound sensitivity: Difficulty tolerating normal levels of stimulation.
Some symptoms might seem mild at first but can grow more serious over time. That’s why even “small” head injuries should be checked out by a doctor.
Early treatment can make a big difference in recovery and in some cases, save a life.
Legacy and long‑term impact
Brain injuries can take away a person’s independence.
Some people have trouble returning to work or school. Others deal with mood swings, depression, or personality changes.
Families often find themselves becoming full-time caregivers, which can be emotionally and financially draining.
Survivors may endure physical disability, speech or motor deficits, memory or executive function impairments, emotional instability, PTSD or depression (PTSD incidence ~15–20% among TBI sufferers).
Family caregivers face emotional and financial strain; lifetime care costs can exceed USD 3 million per severe TBI survivor.
Example: A 35-year-old construction worker suffers a TBI from a fall. He’s unable to focus, gets angry easily, and can’t return to his job. His partner now has to work extra hours and care for their children, all while managing his doctor visits.
Legal challenges in TBI claims
TBI cases aren’t like other personal injury claims. The damage can be invisible. Recovery is unpredictable. Costs are high.
Proving damages requires linking mechanisms of injury with medical findings, prognosis and cost.
Challenges include delayed symptom onset, mild scan results despite cognitive impairment, and disputing secondary injury progression. Insurers may dispute severity or access to long‑term care.
Rare symptoms like PTSD, depression or personality change may complicate quantification of loss.
Claimants must build cases around multidisciplinary evidence: accident reconstructions, medical records, neurology, rehabilitation prognosis, life‑care planning and vocational assessments.
Settlement ranges vary widely: minor concussion may yield modest recovery, while complex, permanent impairments can lead to multi‑million dollar verdicts or settlements.
Demographics and risk groups
Highest risk groups: males (twice female rates), children ages 0–14, young adults (15–24), and adults over 65.
Rates climbed among incarcerated individuals, veterans, people experiencing homelessness, and ethnic minorities.
When to engage a traumatic brain injury lawyer
Consider legal counsel when:
- Immediate medical evidence links another party’s breach to TBI
- Symptoms persist or progress after “mild” injury
- Independence or return to work is compromised
- Insurers dispute coverage, or caregiver and long‑term care costs escalate
- Fault may span more than one party (driver, premises owner, medical provider, manufacturer)
Strong cases rely on documenting accident details, medical follow‑up, expert imaging interpretation, neuropsychological testing, rehabilitation prognosis and family impact. If you're injury was the result of a car accident, check out our lawyer directory.
Final thoughts
Traumatic brain injuries can be life-changing, not just for the person hurt but for their entire family.
They often come with years of recovery, uncertainty, and financial strain.
But you don’t have to face it alone if you don’t want to. While the Mighty.com AI claims helper can handle some aspects of a TBI claim, you may want to consult a lawyer too.
A lawyer who understands the medical and legal side of TBIs can help you get the support you need.
If you’re not sure where to start, Mighty.com’s AI helper or a free consultation is a good first step. It doesn’t cost anything to find out what your rights are and it could make all the difference.
Sources
- National Library of Medicine - The Scope and Burden of Traumatic Brain Injury - https://www.ncbi.nlm.nih.gov/books/NBK580076/
- Wikipedia - Traumatic Brain Injury - https://en.wikipedia.org/wiki/Traumatic_brain_injury
- https://www.ncci.com/Articles/Pages/Insights-Traumatic-Brain-Injuries-WorkersComp.aspx
- National Council on Compensation Insurance - Traumatic Brain Injuries in Workers Compensation - https://www.ncci.com/Articles/Pages/Insights-Traumatic-Brain-Injuries-WorkersComp.aspx
Know Your Claim’s Worth—and Settle It
Serious injury or no injury at all, move your case forward instantly from your phone.
Thank you for submitting your information.

About the author
Joshua is a lawyer and tech entrepreneur who speaks and writes frequently on the civil justice system. Previously, Joshua founded Betterfly, a VC-backed marketplace that reimagined how consumers find local services by connecting them to individuals rather than companies. Betterfly was acquired by Takelessons in 2014. Joshua holds a JD from Emory University, and a BA in Economics and MA in Accounting from the University of Michigan.